This article was written by Jenny To, PhD.
Key points
Below we’ll describe relationships between the oral microbiome, oral health, and digestive diseases.
How the oral and gut microbiomes compare
Although disease changes many aspects of the microbiome, here is a brief overview of how the oral microbiome and gut microbiome generally compare.
Who is there?
The oral microbiome is second only to the gut microbiome in terms of numbers of bacterial species – about 700 species in the oral cavity compared to 500 - 1000 species in the intestinal system. Alongside bacteria, both environments also house an undetermined amount of viruses, fungi, and protozoa. And there are even more species yet to be identified – known as microbial dark matter.
Key bacteria found uniquely in each environment:
In the mouth
In the gut
What are the conditions like?
In the mouth
The oral cavity has many different habitats including gum tissue and plaque below and above the gumline. Along tooth surfaces, oral bacteria assemble highly organized and stable biofilms in the form of dental plaque. Bacteria are also found on the tongue, tonsils, throat, buccal mucosa, hard palate, and importantly – saliva.
Many factors shape these microenvironments in the mouth, including pH, salt level, redox potential, oxygen, and available nutrients. As you’re well aware, dental hygiene also plays a huge role in shaping the oral microbiome.
In the gut
The conditions in the small and large intestines are distinct. In the small intestine, food moves quickly through, is broken down by acids, and its nutrients absorbed. The bacteria in the large intestine are largely comprised of anaerobes, which utilize food that wasn’t digested in the small intestine. Unlike the oral microbiome, the gut microbiome is less stable and more subject to shaping by host and environmental factors. These selective pressures help to maintain homeostasis by forming barriers – described below – between the immune system and microbial infection.
Do oral bacteria colonize the gut?
Not easily in a healthy individual. A comparison of saliva and stool samples taken from the same healthy subjects revealed that the bacterial composition of each sample were very different and distinct. Several other studies also report very little overlap in saliva and stool microbial composition. These bacteria have evolved with humans over time to survive in different conditions in the mouth and gut. If introduced to the gut microbiome, oral bacteria would have to compete for resources and space with native commensal (friendly) bacteria in the gut.
There are several barriers that prevent oral bacteria from setting up shop in a healthy digestive system. These include:
What happens when these barriers break down?
As mentioned above, these barriers prevent most oral bacteria from hanging out and stirring up trouble where they don’t belong in the digestive system. Disease states, inflammation, and even medication, however, can disrupt these barriers and make it easier for oral microbes to influence disease in the gut.
Here we highlight major and emerging GI disorders with relevant studies exploring relationships with the oral microbiome.
Inflammatory Bowel Disease (IBD)
IBD is characterized by chronic inflammation which damages the GI tract over time. Where and how the damage occurs determines if it is ulcerative colitis (continuous damage usually starting in the rectum into the colon) or Crohn’s disease (patchy damage affecting any part of the GI tract).
Recurrent canker sores (aphthous ulcers) in the mouth are often the first sign of Crohn’s disease. Speak to your dentist and doctor if you have concerns about GI disorders and also frequently experience canker sores.
Many studies have described increased comorbidity (co-presence) of gum disease and IBD. One meta-analysis reported 30% higher risk of periodontitis in patients with IBD than in control subjects without IBD.
But how does gum disease and oral microbes influence IBD? One recently proposed model describes how oral species may not only translocate to the gut but expand and make gut inflammation worse.
In one experiment, mice with colitis were fed specific species of oral bacteria to observe the effect on their colitis. This study found that periodontitis (severe gum disease) worsens gut inflammation in two ways. First, periodontitis leads to an increase of harmful oral bacteria. These bacteria are then swallowed and trigger gut inflammation. In the study, specific Klebsiella and Enterobacter species translocated from the oral cavity to the gut and triggered gut inflammation, while other species such as Streptococcus salivarius did not.
Second, periodontitis also leads to generation of specific immune cells, called Th17 cells, in response to growing oral bacterial infection in the mouth. When we’re healthy, Th17 cells protect against infection by engaging pro-inflammatory pathways. But as they accumulate in the oral cavity, they can then circulate through the bloodstream to the intestine, inducing excessive inflammation. The study found that the Th17 cells – made from oral infection in the mouth – moved to the gut and reunited with translocated oral bacteria. Because these Th17 cells were designed to mount an inflammatory response against oral bacteria, inflammation in the gut was made worse.
Although we emphasize the link between gum disease and IBD, dental cavities (caries) may also be related to IBD. Patients with Crohn’s have been found to have higher measures of cavities and higher levels of salivary Lactobacillus and Streptococcus mutans – two bacteria associated with cavity formation – compared to people without Crohn’s. This relationship is still not well understood, but diet may likely play an important role in both these conditions.
Small intestinal bacterial overgrowth (SIBO)
Another GI disorder gaining more recognition is small intestinal bacterial overgrowth, or SIBO. Despite growing awareness, SIBO is still poorly understood. It isn’t yet precisely or consistently defined in the clinic. However, it is generally attributed to abnormal changes in the number and the types of bacteria found in the small intestine.
Many of these bacteria aren’t usually found in this part of the digestive tract. Because of the presence of bile (digestive juices) and how rapidly food content moves through, a healthy small intestine doesn’t house a large number of bacteria – unlike the large intestine. An overgrowth of bacteria collecting where they don’t belong leads to blockages preventing food from moving through the small intestine normally. Food stopped at these blockages prevents sufferers from digesting vital nutrients (malabsorption) and also feeds the bacteria. Presented with a buffet and no reason to leave, these bacteria continue to grow in numbers and contribute to chronic GI issues.
A patient suspected of suffering from SIBO may be diagnosed by either a breath test or by collecting a fresh bacterial sample and counting the number of live bacteria. But these methods can be challenging to perform and interpret. Using genomic approaches, like next-generation sequencing, to analyze the small intestine microbiome in SIBO and other GI disorders will be critical to understand what bacteria are present and what they are doing.
Although there are limited studies specifically identifying oral bacteria contributing to SIBO, the possibility of swallowed oral bacteria finding their way to these blockages and impacting immune responses in the small intestine cannot be ruled out.
In one study, researchers found that feeding live oral P. gingivalis, L. bacillus, and S. salivarius to mice lowered levels of Th17 cells in the small intestine. As mentioned above, Th17 cells are important in mounting an immune response against bacterial infections. If the immune system can’t produce enough Th17 cells to respond to the infection, this bacteria can overgrow and overstay in the small intestine.
Moreover, some evidence has shown that people diagnosed with SIBO (and a related condition, functional dyspepsia) have not only altered oral microbiomes compared to healthy people but also more severe periodontal disease measurements, suggesting that these digestive disorders possibly influence oral health.
Colorectal cancer
Gum disease is increasingly linked to colorectal cancer. A recent study showed that the rate of new colorectal cancer diagnoses among participants who had a history of periodontal disease was nearly 50% higher than those who had no history of periodontal disease.
The most strongly implicated cancer-causing oral microbe is F. nucleatum, which is not typically found in a healthy gut. For a deeper dive on how oral microbe F. nucleatum drives colorectal cancer development, read our previous articles – Cancer and Your Oral Microbiome and Fusobacterium nucleatum in Colorectal Cancer: What You Need to Know.
How to improve oral & gut health
Diet
What and how we eat have a major impact on oral health. Fortunately, some of the same beneficial dietary choices for oral health can also benefit gut health.
Oral health
Poor oral health can make it hard to properly chew and prepare food for digestion in the gut, leading to gastrointestinal problems. Inflammation in the mouth and an overgrowth of harmful oral bacteria can make these problems worse. While there is still emerging research unraveling the relationship between the oral microbiome and systemic diseases – like digestive disorders – we think a great way to start improving your overall health is to take steps to boost your oral health.
Interested in learning more?
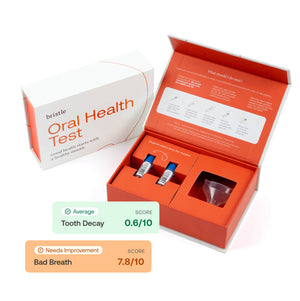
The Bristle Oral Health Test analyzes the levels of good and bad bacteria in your saliva and gives you recommendations to improve your health. Our gut inflammation score will also show you the abundance of bacteria associated with gut health in your saliva. Through actionable, personalized recommendations, you can take immediate steps to improve your oral — and overall – health.