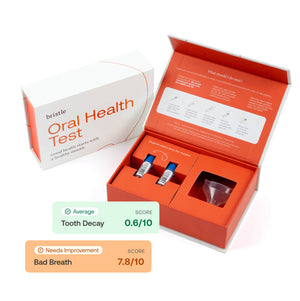
Bristle Comprehensive Oral Health Test
Bristle has developed a convenient low-cost state-of-the-art salivary test, leveraging next-generation sequencing of the oral microbiome, which can inform on the risk of periodontal disease and dental caries.
Executive Summary
Introduction
Oral diseases such as periodontal disease and dental caries are among the most common diseases in the world. The CDC estimates that 47.2% of the general population for individuals over 30, and 70.1% for individuals over 65 have gum disease (2). Recent studies have identified an association between microbes in the mouth and an increased prevalence of oral diseases (periodontal disease and caries) (3). This association creates an opportunity to introduce a new form of oral health screening and treatment using microbiome testing to identify and proactively treat individuals with potentially harmful bacteria. Importantly, preventive treatments have been shown to mitigate the progression of both gum disease and dental caries when applied in the early stages of disease, illustrating the importance of early detection of disease (4).
The oral microbiome in oral disease
The oral microbiome is a dynamic and complex community of bacteria, fungi, and viruses that can influence oral health and disease. Specific species of bacteria have been shown to be causally linked to the progression of dental caries and periodontal disease (3). For example, dental caries usually occur when sugar is metabolized by specific types of bacteria, such as Streptococcus mutans and Lactobacillus species, in the mouth to produce acid, resulting in dental demineralization (1). Similarly, key microbial species such as Porphyromonas gingivalis, Tannerella forsythia, and Treponema denticola, are known periodontal pathogens, and their abundance is linked to periodontitis (5). Furthermore, dozens of other bacterial species have been associated with the progressive stages of periodontal disease, such as Eubacterium brachy and Aggregatibacter actinomycetemcomitans (6,7). Importantly, while single bacterial species have been associated with disease, oral health status is influenced by the entire oral microbiome (hundreds of microbial strains), driving the importance of comprehensive profiling of the oral microbiome to assess health status (11). Finally, the oral microbiome also harbors culturable commensal bacterial species that may reduce the incidence and progression of tooth decay and gum disease (12, 13).
The role of oral health in systemic health
Gum health has also been shown to play a major role in systemic health. Periodontal disease is associated with adverse outcomes for pregnancy, diabetes, cardiovascular disease, arthritis, and neurological diseases (8). For example, periodontal disease increases a patient's lifetime risk of cardiovascular disease by 19%. In patients 65 years and older, the increased relative risk is as high as 44% (8). Early detection and active management of periodontal disease is therefore critical to improving overall health.
Test development and validation
Study design
The purpose of this study was to assess the accuracy of the Bristle platform to classify dental caries and periodontal disease based solely on the composition of the salivary oral microbiome. One hundred adult patients (18 years or older) were recruited at the University of the Pacific Dugoni Dental school to participate in a research study, where they were evaluated for cavities by radiography, visual inspection, or tactile probing, and for periodontal disease by pocket depth. Periodontal disease was defined as pocket depth >4mm at any single position. Unstimulated patient saliva was collected prior to any treatment or dental cleaning.
Laboratory procedures
The Bristle metagenomic library prep to comprehensively profile the oral microbiome is based on laboratory products from industry leaders such as Illumina, Zymo Research, and New England Biolabs. Total genomic DNA was extracted from the samples using a Zymobiomics DNA isolation kit. DNA was quality controlled to ensure high-quality DNA isolation. Purified DNA was subjected to in-house library preparation methods to generate Illumina sequencing libraries, which were quality controlled by fragment analysis and pooled equimolar for sequencing. Pooled libraries were sequenced on a NovaSeq to at least 5 million paired-end reads per sample at 150bp length.
Bioinformatics
The Bristle bioinformatics pipeline was built using well-established algorithms leveraged worldwide in academic and commercial labs. Fastqs were downsampled by seqtk to 5M reads and aligned to a human genome reference sequence (hg38) to remove human reads. The remaining reads were subject to Bristle's proprietary bioinformatics workflow to identify and quantify the relative abundance of bacterial species. In short, raw sequencing data was mapped to over 30,000 bacterial reference genomes to measure the relative abundance of bacterial strains, including those classified as periodontal and dental caries pathogens. A Bristle algorithm, which takes into consideration the relative abundance of each bacterial strain, was used to compute a risk score for both caries and gum disease. The Bristle algorithm weighs the abundance of disease and healthy associated bacterial strains backed by internal studies and peer-reviewed research articles.
Accuracy Results
We assessed the accuracy of our classification algorithm through a receiver-operating curve, which is summarized here as an area under the curve (AUC). An AUC of 1.0 is perfect at discriminating between classes, while an AUC of 0.5 is essentially random.
The Bristle Comprehensive Oral Microbiome Test achieves an AUC = 0.88, with 74% sensitivity and 85% specificity for periodontal disease (Figure 1A) and an AUC = 0.81, with 69% sensitivity and 75% specificity for dental caries (Figure 1B). To date, this data demonstrates that the Bristle microbiome test exhibits best-in-class sensitivity and specificity for an oral health salivary microbiome test.


Conclusion
Our validation study demonstrates the utility and accuracy of the Bristle oral microbiome test in assessing risk for caries and gum disease. Our test is supported by decades of research that has supported the role of the oral microbiome in driving oral disease. Additionally, the latest research and theories suggest that the oral microbiome is responsible for maintaining oral health. Analyzing both the beneficial and virulent microbes grants increased resolution in the microbial-based assessment of oral health status (11).
The Bristle comprehensive oral microbiome test is not only sensitive and specific, but also allows for practitioners to remotely connect with patients through objective, data-driven insights into oral health status.